Covid-19 Vaccine Information
Dr.Somchai Leelasiriwong and
Dr.Raweerat Sitcharungsi
With a wealth of information regarding COVID-19 vaccines being available, it may be hard to discern the facts. Therefore we have sourced the important information for ease of access. Topics covered include “Should we hurry to get the vaccine?”, “Can I have an injection if I have a congenital disease?”, “What risks or side effects should I be aware of?” etc. This will allow everyone to be properly educated, before making the decision.
Contents
- Observations on the current COVID 19 vaccine
- Who should get the COVID-19 vaccine injection first?
- Who is not yet recommended for COVID-19 vaccination?
- Can COVID-19 vaccine prevent us from getting infected with COVID?
- Instruction after the COVID-19 vaccination.
- Side effects of the Covid 19 vaccine that have been seen
- How long will the immunity from the COVID-19 vaccine exist in the body?
- The four main types of COVID 19 vaccine
- How many brands of the COVID-19 vaccine are there in Thailand? What techniques are used in production?
- Common mild side effects after COVID-19 vaccination
- What kind of side effects that the injection of second dose should not be done
- Conclusion
Observations on the current COVID 19 vaccine
- Covid-19 vaccine is the most effective way in preventing covid-19 disease: Not only the vaccines can decrease the number of Covid19 patients, but it also reduce the chance of severe morbidity and death from Covid19 infection.
- Single injection is more convenient: Johnson & Johnson and CanSino Biologics are the most interested vaccines because it can save the patient’s time. Johnson & Johnson and CanSino Biologics will be administered only 1 time.
- COVID-19 vaccine (mRNA type): This is a vaccine that uses a new technique, which allows easy and fast production. It is also convenient to be modified for more variants of the virus. However, the mRNA type of COVID-19 vaccine also has limitation in storage and transportation as weakness, because the mRNA type of COVID-19 vaccine need to be stored in very low temperature, especially Pfizer which need to be stored in the container with a temperature of at least -70 ˚C. Comparison between another brand of this type of COVID-19 vaccine, Moderna vaccine seems to be less complicate in storage and transportation, because can be stored in the temperature only 2 -8 ˚C (with validation of 30 days)
- The Novavax Vaccine is quite safe for immune compromised patients .The Novavax Vaccine is made from component of proteins from the virus and produced from dead strains such as Sinovac, Sinopharm, and Covaxin . The components of the vaccine have no risk for infection and it is advised for immune compromised patients.
- Inactivated Covid-19 vaccines, for example Sinopharm, have high cost of production. The virus has to be kept in a high-level laboratory culture (Biosafety level 3). Therefore, the production of this type of Covid-19 vaccine has high cost which lead this vaccine to be more expensive than other vaccines as well.
Who should get the COVID-19 vaccine injection first?
Because Covid19-vaccines are not available for all Thai people currently, prioritizing on the groups that should be vaccinated first must be considered. The elderly and people with severe co morbidity have more mortality with Covid-19. Therefore, they must be prioritized first.
Moreover, with the purpose of reducing morbidity, mortality, and hospitalization rate, the target groups that should be vaccinated first according to the Ministry of Thai Public Health are as followed:-
1. Medical and public health personals in both public and private sectors.
2. People with underlying disease, especially diseases with various chronic conditions or in the risk groups that are:-
2.1 Chronic respiratory disease
2.2 Cardiovascular disease
2.3 Chronic kidney disease
2.4 Cerebrovascular disease
2.5 All types of cancer
2.6 Diabetes Mellitus
2.7 Obesity (Updated on May 1, 2021)
3. Elderly people whose aged 60 years old and over.
4. Officers involved in the control of COVID-19, such as village health volunteers, military and police officers.
Who is not yet recommended for COVID-19 vaccination?

Children
COVID-19 vaccination is not recommended for children, because the vaccine is currently approved only for individuals 18 years of age and older, except for Pfizer-BioNTech, which has been expanded by the US FDA for adolescent 16-18 years of age. However, the study found that children have mild symptoms.
Those who need medical consultation before vaccination.
– People with underlying illnesses whose symptoms remain unstable and critical
– People receiving high-dose immunosuppressant
– People taking anticoagulants (warfarin)
Can COVID-19 vaccine prevent us from getting infected with COVID?
The overall effectiveness of disease prevention is divided into two forms: effective prevention of asymptomatic COVID 19 and effective prevention of symptomatic COVID 19.
The effectiveness of vaccines in news report, such as the 95% effectiveness of Pfizer vaccine, is actually the effectiveness of the symptomatic disease prevention. However, the effectiveness of asymptomatic disease prevention is mostly unknown.
Therefore, it can be concluded that at present the vaccine is not 100% protected against infection. People who have been injected may still have a chance of getting the disease. But the vaccine can reduce complications, hospitalization and deaths.
Instruction after the COVID-19 vaccination.
Wait for 30 minutes after the injection, do not go anywhere: The anaphylaxis usually occur within 15-30 minute after vaccine administration. Therefore, 30-minutes observation after vaccinated at administration area is mandatory.
Social distance and personal hygiene is still obligatory: you still have to wash hand with soap or alcohol, keep distance, and wear a mask, in order to prevent COVID-19 infection.
Side effects of the Covid 19 vaccine that have been seen
Side effects
Some of serious side effects have been reported with COVID-19, including:-
Thromboembolic conditions
– The case of AstraZeneca: The European Medical Agency (EMA) announced that it is possible that the AstraZeneca vaccine may be linked to vaccine induced thrombotic thrombocytopenia or VITT after it was found that some people suffered from thromboembolic conditions after the first dose of the vaccines. There were even reports of death case from VITT; however, it is important to remember that the risks of dying or suffering severe outcomes from COVID-19 remain far greater than the risk following AstraZeneca vaccine.
It is advisable for people to get this vaccine that if you have severe headaches, blurred vision, chest pain, trouble breathing, swollen legs, ongoing abdominal pain and spots of bleeding on the skin, you shall immediately consult a doctor.
– The Johnson & Johnson case: There were suspected cases of vaccine-induced thrombotic thrombocytopenia after patients received the Johnson & Johnson COVID-19 vaccine within 1-3 weeks. Some countries have decided to stop using J&J vaccines.
Are there any other serious side effects?
– Astra Zeneca: Besides of thromboembolic issues, AstraZeneca vaccine has been reported to cause other severe side effects, such as fever above 40 ˚C, and a patient with myelitis after receiving a second dose.
– BioNTech/Pfizer: It was reported that only 4.7 out of 1 million people who were injected the vaccine, would have severe allergic reaction. However, according to USA, there was no one who has had serious side effects which lead to the death.
– Moderna: It was reported that only 2.5 out of 1 million people who were injected the vaccine, would have severe allergic reaction. So far, the United States has no report of direct deaths from vaccination.
– Sinovac, Novavax and Sputnik V: Phase 3 of the studies has not reported any serious adverse reactions.
In conclusion, serious reaction, such as vaccine induced vaccine induced thrombotic thrombocytopenia is extremely rare. Moreover, anaphylaxis rates are similar for COVID-19 and other common vaccines.
How long will the immunity from the COVID-19 vaccine exist in the body?
A preliminary study by the La Jolla Institute for Immunology found that vaccines could provide protection against disease for at least 6 months, depending on the individual’s body. Besides the study, still there is no any information to officially support the existing time of immunity in the body. However, it is recommended to complete 2 doses of vaccinations (also depend on each type of vaccine) for the most effective immunity in the body.
The four main types of COVID 19 vaccine
Nowadays, there are four main types of vaccines used to prevent COVID-19. They are divided based on the techniques in the production:
– Genetic material COVID-19 vaccine type of (mRNA vaccines) is a new technology that was used to develop vaccines against Ebola. In the case of COVID-19, the vaccine is made by using the genetic material of the SARS-CoV-2 virus (SARS-CoV-2), which, when injected into the body, mRNA directly produced spike protein of the virus. This type of virus will cause the body to build an immune response to this virus.
There are currently two companies using this technology: BioNTech/Pfizer and Moderna
– COVID-19 vaccines that use viral vector. Viral vector is a weakened virus. Thus, it cannot make us sick. Researchers then deposit the genetic material of the SARS-COV-2 virus (SARS-CoV-2) into the viral vector. After receiving the vaccine, the body creates an immune response to the SARS-COV-2 virus. This type of vaccine is effective because it can mimic the natural infection.
Johnson & Johnson’s, Oxford – AstraZeneca’s and Sputnik V’s vaccines use this technique.
– COVID-19 vaccine that made from a part of the virus (Protein-based vaccines). The researchers took some proteins of the SARS-CoV-2 virus (SARS-CoV-2), such as spike protein, and then mixed it with an immune stimulant. When injected, it will stimulate the body to build an immune system against the virus. This technique has been used for a long time, because, it is a technique that used to produce influenza and hepatitis B vaccines.
A vaccine company that uses such a technique is Novavax and etc.
– COVID-19 vaccine of inactivated vaccines type is produced from the SARS-CoV-2 virus that has been killed by chemicals or heat. When injected into the body, it will stimulate the body to build immunity to the virus. This is a technique previously used in the production of the hepatitis A or the polio vaccines (injectable), but, because it must be done in a level 3 laboratory. Therefore, the production is slow and has high costs.
The vaccines that use this technique are Sinovac and Sinopharm
How many brands of the COVID-19 vaccine are there in Thailand? What techniques are used in production?
The currently available vaccine in Thailand has been approved by both the Thai Food and Drug Administration (FDA), and the World Health Organization, including AstraZeneca and Sinovac vaccine (Latest update, April 21, 2021).

AstraZeneca
This is a Viral Vector vaccine for injection to people of aged 18 years old and over. It will be injected into the upper arm, a total of 2 doses; each dose injects 10-12 weeks apart.
Sinovac
It is the inactivated vaccine for injection in people of aged between 18 – 59 years old. It will be injected in the upper arm for 2 doses. The Immunization Subcommittee guides that each needle must be injected between 2 to 4 weeks apart, except for those in severe epidemic areas that will be given each injection 2 weeks apart.
Currently, Thailand is urgently contacting other vaccine manufacturers and the progress is under negotiation.
Common mild side effects after COVID-19 vaccination
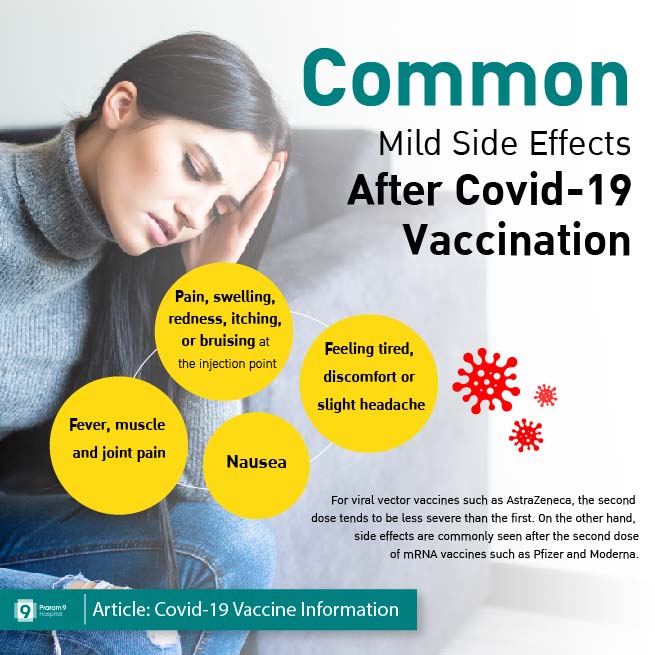
• Pain, swelling, redness, itching, or bruising at the injection point.
• Feeling tired, discomfort or slight headache.
• Fever, muscle and joint pain
• Nausea
Viral vector vaccines type, AstraZeneca, for example, the second dose tends to be less severe than the first. On the other hand, the mRNA type such as, Pfizer and Moderna, side effects are commonly seen after the second dose.
In Thailand up to May 2021, over a million people have been vaccinated at least one dose. The adverse reactions reported were mild and transient. Nevertheless, there was a report of immunization related focal neurological syndrome after injection with Sinovac vaccine. The incidence is roughly 5 in 10,000 people vaccinated. The symptom is transient numbness and mild weakness. None of them have abnormality in magnetic resonance imaging of brains.
What kind of side effects that the injection of second dose should not be done
It is suggested not to receive a second dose if you have an allergic reaction to the COVID 19 vaccine immediately after the injection:
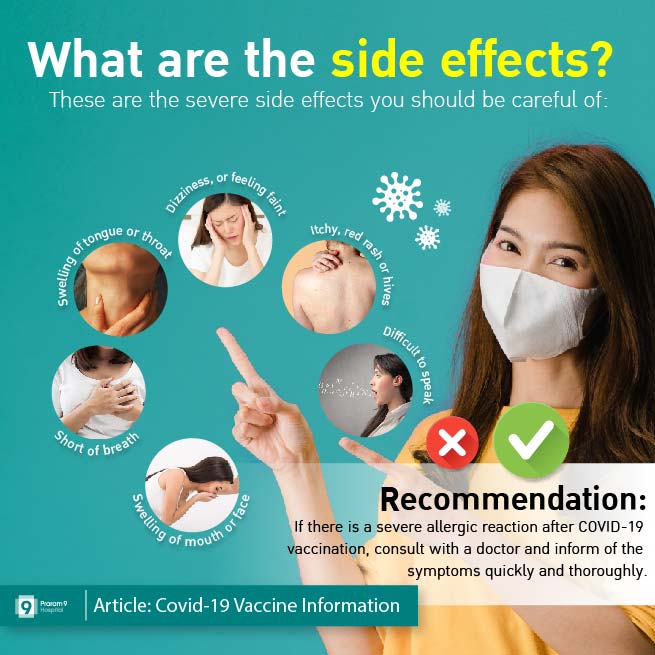
· Itchy, red rash or hives
· Swollen of mouth, tongue, face, or throat
· Nausea and vomiting
· Dizziness, flaring, low blood pressure or tachycardia
· Difficulty breathing, gasping of breath or stuffy nose
· Difficult to speak
Conclusion
Everyone is encouraged to get vaccinated for COVID19 as the benefits far outweigh the risk.
For high risk people, they should be vaccinated immediately in order to reduce the chance of infection, severe morbidity and mortality.
However, Pregnant women (or planning to become pregnant), immunocompromised patients, patients on immunosuppressive medication and patients on anticoagulants; these group of people should always consult doctors before vaccinated.
Thailand is currently in negotiations to acquire vaccines from Pfizer and Moderna, in order to get more vaccination options in the future. Hopefully, the epidemic situation will be better soon. Please follow the news via Praram 9 Hospital International Facebook. Praram 9 hospital would like to send our encouragement to everyone encounter difficulties during this time.