Health Articles
Knowledge
Hepatitis
By Dr. Rapeepun Kalayavinai
28th July is World Hepatitis Day. Understanding the different forms of hepatitis, who is at risk and how it can be prevented and treated can be valuable to protect you and your loved ones from the disease.
Hepatitis is an inflammation of the liver that is caused by a variety of infectious viruses and noninfectious agents leading to a range of health problems, some of which can be fatal. There are five main strains of the hepatitis virus, referred to as types A, B, C, D and E. To this day, viral hepatitis remains a major public health problem in Thailand. Chronic infection with hepatitis B and C viruses are the leading causes of chronic liver diseases, including cirrhosis and hepatocellular carcinoma (HCC).
Symptoms of viral hepatitis
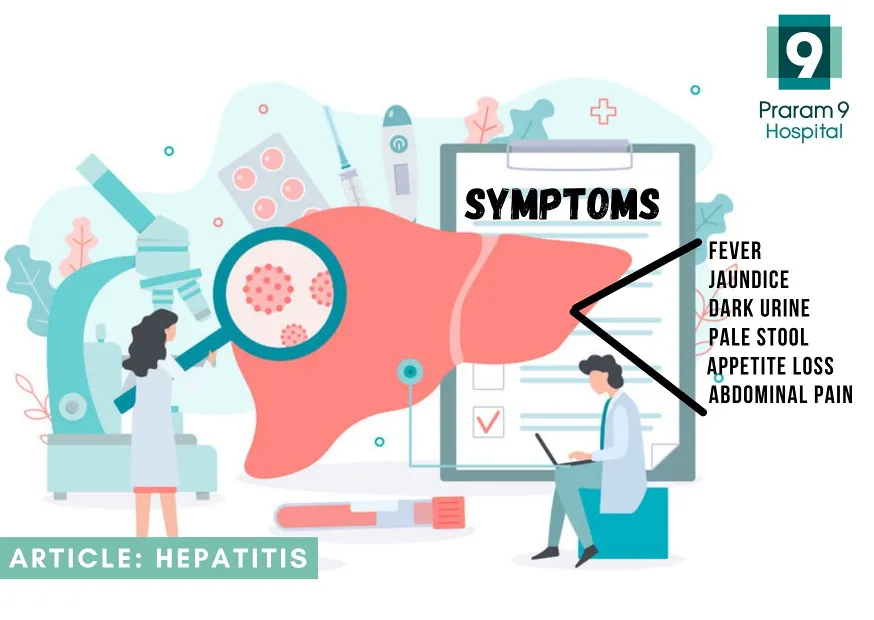
Symptoms and severity of viral hepatitis varies. Short-term (acute) hepatitis often has no noticeable symptoms, so you may not realise you have it. If symptoms do develop, they can include:
- a high temperature
- loss of appetite
- abdominal pain
- dark urine
- pale, grey-coloured feces
- itchy skin
- yellowing of the eyes and skin (jaundice)
Long-term (chronic) hepatitis also may not have any obvious symptoms until the liver stops working properly (liver failure) and may only be picked up during blood tests. In the later stages, chronic hepatitis can cause liver cirrhosis, or scarring of the liver, which manifest as jaundice, swelling in the legs, ankles and feet, confusion, and blood in your stools or vomit. Some people with chronic hepatitis may go on to develop liver cancer.
What you need to know about Hepatitis A, B and C

Hepatitis A
Hepatitis A is most likely contracted from contaminated food, water or someone already infected. Prior to the 1980’s, hepatitis A virus (HAV) infection was the most common cause of acute viral hepatitis in Thailand, especially in children younger than 6 years of age. It has shifted from high to low endemicity as a result of Thailand’s improving sanitation, socioeconomic status, and education. Thailand achieved low to very low endemicity for hepatitis A.
The lack of prior HAV exposure and immunity is a significant concern for potential outbreaks and symptomatic infection in adolescents, and those with advanced age and weakened immune system. Either an inactivated or a live-attenuated HAV vaccine provides very good efficacy with lasting induced immunity. However, the relatively high cost of the HAV vaccine limits its use and is not included in the Expanded Program on Immunization (EPI).
Mild cases of hepatitis A infection do not require treatment, and most who have the infection recover completely with no permanent liver damage. Practicing good hand hygiene is one of the best ways to protect against hepatitis A.
Hepatitis B
Hepatitis B can be either acute or chronic. For some people, chronic hepatitis B infection can lead to liver failure, liver cancer or cirrhosis. It is spread through bodily fluids and blood. Most people infected as adults recover fully, even if their signs and symptoms are severe. Infants and children are much more likely to develop a chronic hepatitis B infection. Thailand is an endemic area of viral hepatitis B. Many Thai people who are infected with viral hepatitis B, don’t know they have infection until they encounter blood screening.
Although no cure exists for hepatitis B, treatment options are available and a vaccine can prevent the disease. Vaccination is recommended for infants; children who weren’t vaccinated in infancy; people being treated for a sexually transmitted infection; health care workers and others who come in contact with blood on the job; people with end-stage kidney disease; and people traveling to areas with high rates of hepatitis B, among others. If a person is already infected, taking certain precautions can help prevent the spread of hepatitis B to others. Although hepatitis B vaccination is included in Thailand Extended Program on Immunization, high risk people as mentioned above, should be screened for viral hepatitis B and viral hepatitis B immunity.
Hepatitis C
Hepatitis C: Most people infected with the hepatitis C virus have no symptoms. And most don’t know they have the hepatitis C infection until liver damage shows up decades later during routine medical tests. Generally considered to be among the most serious of the three viruses, hepatitis C is passed through contact with contaminated blood — most commonly through needles shared during illegal drug use. Hepatitis C infection is treated with antiviral medications intended to clear the virus from the body.
Hepatitis C infection can be asymptomatic for decades but typically appears as liver problems over time. This can happen faster if immune systems decline due to other conditions as they age. The Centers for Disease Control and Prevention (CDC) recommends hepatitis C screening for all baby boomers.
Key facts about viral hepatitis
Key facts
How long does it last?
Hepatitis A : Hepatitis A can last from a few weeks to several months.
Hepatitis B : Hepatitis B can range from a mild illness, lasting a few weeks, to a life-long condition. More than 90% of unimmunized infants who get infected develop a chronic infection, but 10% of older children and adults who get infected develop chronic hepatitis B.
Hepatitis C : Hepatitis C can range from a mild illness, lasting a few weeks, to a serious, life-long (chronic) infection. Most people who get infected with the hepatitis C virus develop chronic hepatitis C.
How is it spread?
Hepatitis A : Via fecal-oral route. i.e. Hepatitis A is spread when a person ingests fecal matter even in microscopic amounts from an infected person.
Hepatitis B : Via blood and body fluids; including
- Birth to an infected mother
- Sex with an infected person
- Sharing equipment that has been contaminated with blood from an infected person, such as needles, syringes, and even medical equipment, such as glucose monitors
- Sharing personal items such as toothbrushes or razors Poor infection control has resulted in outbreaks in health care facilities
Hepatitis C : Via blood including;
- Sharing equipment that has been contaminated with blood from an infected person, such as needles and syringes
- Receiving a blood transfusion or organ transplant before 1992 (when widespread screening virtually eliminated hepatitis C from the blood supply)
- Poor infection control has resulted in outbreaks in health care facilities
- Birth to an infected mother
Who should be vaccinated?
Hepatitis A :
- Children (not included in Thailand EPI)
- All children aged 12–23 months
- All children and adolescents 2–18 years of age who have not previously received hepatitis A vaccine (known as “catch up” vaccination)
- People at increased risk for hepatitis A
- International travelers
- People at increased risk for severe disease from hepatitis A infection
- People with chronic liver disease, including hepatitis B and hepatitis C
- People with HIV
- Other people recommended for vaccination
- Pregnant women at risk for hepatitis A or risk for severe
- Outcome from hepatitis A infection
- Any person who requests vaccination
Hepatitis B :
- All infants
- All children and adolescents younger than 19 years of age who have not been vaccinated
- People at risk for infection by sexual exposure including: people whose sex partners have hepatitis B, sexually active people who are not in a long-term, mutually monogamous relationship, people seeking evaluation or treatment for an STD, and men who have sex with men
- People at risk for infection by exposure to blood including: people who inject drugs, people who live with a person who has hepatitis B, residents and staff of facilities for developmentally disabled people, health care and public safety workers at risk for exposure to blood or blood-contaminated body fluids on the job
- Hemodialysis patients and predialysis, peritoneal dialysis, and home dialysis patients
- People with diabetes aged 19–59 years; people with diabetes aged 60 or older should ask their doctor.
- International travelers to countries where hepatitis B is common
- People with hepatitis C
- People with chronic liver disease
- People with HIV
- People who are in jail or prison
- All other people seeking protection from hepatitis B virus infection
Hepatitis C : There is no vaccine available for hepatitis
How serious is it?
Hepatitis A :
- People can be sick for a few weeks to a few months
- Most recover with no lasting liver damage
- Although very rare, death can occur
Hepatitis B :
15%–25% of chronically infected people develop chronic liver disease, including cirrhosis, liver failure, or liver cancer
Hepatitis C :
- More than 50% of people who get infected with the hepatitis C virus develop a chronic infection
- 5%-25% of people with chronic hepatitis C develop cirrhosis over 10–20 years
Treatment
Hepatitis A : Supportive treatment for symptoms
Hepatitis B : Acute: No medication available; best addressed through supportive care Chronic: Regular monitoring for signs of liver disease progression; some patients are treated with antiviral drugs
Hepatitis C : Acute: There is no recommended treatment for acute hepatitis C. People should be considered for treatment if their infection becomes chronic. Chronic: There are several medications available to treat chronic hepatitis C. Current treatments usually involve 8-12 weeks of oral therapy (pills) and cure over 90% of people with few side effects
Who should be tested?
Hepatitis A : Testing for hepatitis A is not routinely recommended.
Hepatitis B : CDC recommends hepatitis B testing for:
- People born in countries with 2% or higher HBV prevalence, including Thailand
- Men who have sex with men
- People who inject drugs
- People with HIV
- Household and sexual contacts of people with hepatitis B
- People requiring immunosuppressive therapy
- People with end-stage renal disease (including hemodialysis patients)
- People with hepatitis C
- People with elevated ALT levels
- Pregnant women
- Infants born to HBV-infected mothers
Hepatitis C : CDC recommends hepatitis C testing for:
- All adults aged 18 years and older
- All pregnant women during each pregnancy
- People who ever injected drugs and shared needles, syringes, or other drug preparation equipment.
- People with HIV
- People who have ever received maintenance hemodialysis. Regular testing is recommended for people who currently receive maintenance hemodialysis.
- People with persistently abnormal ALT levels
- People who received clotting factor concentrates produced before 1987
- People who received a transfusion of blood or blood components before July 1992
- People who received an organ transplant before July 1992
- People who were notified that they received blood from a donor who later tested positive for HCV infection
- Health care, emergency medical, and public safety personnel after needle sticks, sharps, or mucosal exposures to HCV‑positive blood
- Children born to mothers with HCV infection
- Any person who requests hepatitis C testing should receive it.
Reference
- Nawarat Posuwan, Nasamon Wanlapakorn, Palittiya Sintusek, Rujipat Wasitthankasem, Kittiyod Poovorawan, Sompong Vongpunsawad, Yong Poovorawan, Towards the elimination of viral hepatitis in Thailand by the year 2030, Journal of Virus Eradication Volume 6, Issue 3, 2020
- https://www.infectioncontroltoday.com/view/abcs-hepatitis-mayo-clinic-expert-explains-types-prevention
- https://www.nhs.uk/conditions/hepatitis/
- https://www.cdc.gov/hepatitis/abc/index.htm
About the Author