Health Articles
Knowledge
Bariatric Surgery
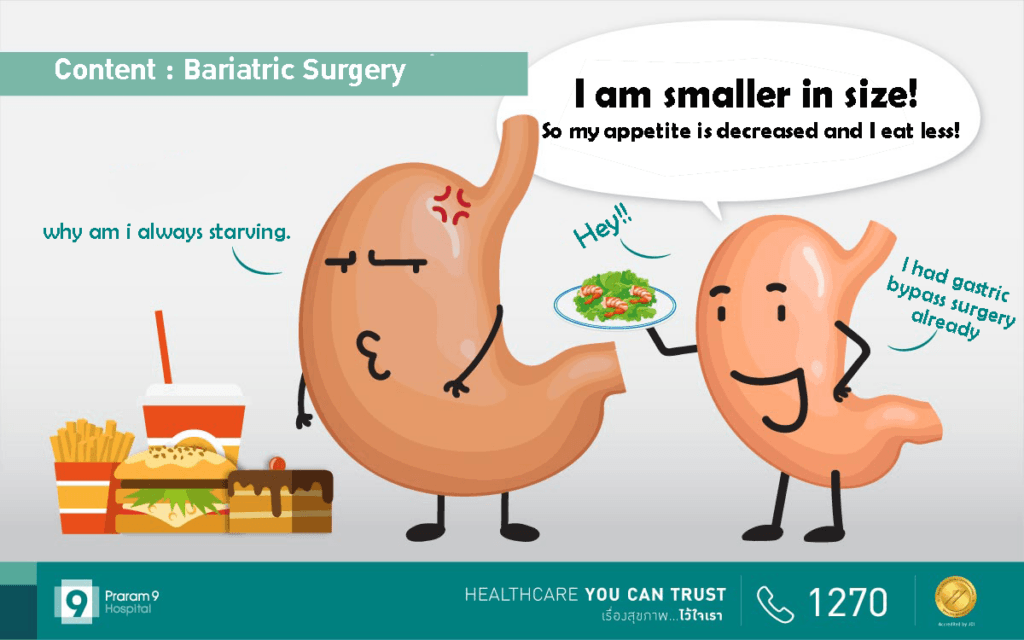
Obesity has become an epidemic of global proportions. Many people are living with a high risk of dying from complications of their obese status, or living with a disability and/or a psychosocial stigma that prevents them from enjoying a satisfying life. The general recommendation to morbidly obese patients to lose 10% of their initial body weight, is well known to have a positive impact and therefore reducing their cardiovascular risk.
Conventional obesity management such as diet
control and exercise has limitations in patients with morbid obesity. Weight loss surgery, therefore, is another
option to lose weight in morbidly obese patients. Weight loss surgery, also
known as bariatric surgery, can lead to significant weight loss and help
improve or even cure many obesity-related conditions, such as type 2 diabetes or high blood pressure.
Content:
- What is bariatric surgery?
- Who is a candidate for weight loss surgery?
- How to diagnose obesity?
- How does obesity harm your health?
- Why do conventional lifestyle interventions not help in morbid obesity?
- How many types of bariatric surgery are there?
- Dietary guidelines after bariatric surgery
- Complication of bariatric surgery
- Is it possible to gain back weight after bariatric surgery?
- Summary
What is bariatric surgery?
Gastric bypass and other weight-loss surgeries — known collectively as bariatric surgery — involve making changes to your digestive system to help you lose weight. Bariatric surgery is done when diet and exercise haven’t worked or when you have serious health problems because of your weight. Some procedures limit how much you can eat. Other procedures work by reducing the body’s ability to absorb nutrients. There are also other procedures which can do both.
It is now clear that caloric restriction per se does not explain all the reduction in stored fat mass after surgery. A number of gastrointestinal hormones, including glucagon-like peptide (GLP)-1, peptide YY, oxyntomodulin, GLP-2, glucose-dependent insulinotropic polypeptide, ghrelin etc., can play roles in energy homeostasis and could be involved in bariatric surgery-related weight loss and weight loss maintenance.
Who is a candidate for weight loss surgery?
Indications for bariatric surgery for people with Asian ethnicity is BMI >37 or BMI >32.5 with T2DM or two significant obesity related co-morbidities.
(Source: Asia Pacific Metabolic and Bariatric Surgery Society (APMBSS: 2005), https://ebrary.net/102191/health/asia_specific_guidelines
Qualifications for bariatric surgery in people with European or American descendents include:
- BMI ≥ 40, or more than 100 pounds overweight.
- BMI ≥ 35 and at least one or more obesity-related co-morbidities such as type II diabetes (T2DM), hypertension, sleep apnea and other respiratory disorders, non-alcoholic fatty liver disease, osteoarthritis, lipid abnormalities, gastrointestinal disorders, or heart disease.
- Inability to achieve a healthy weight loss sustained for a period of time with prior weight loss efforts.
For example, an adult who is 5’11″ tall and weighs 290 lbs would have a BMI over 40. Calculate your BMI. – https://asmbs.org/patients/who-is-a-candidate-for-bariatric-surgery
How to diagnose obesity?
Obesity is diagnosed when your body mass index (BMI) is 30 or higher. To determine your body mass index, divide your weight in kilograms by your height in meters squared. Calculate your BMI.
About the Author